“Women suffer much more from chronic pain and pain disorders than men. The reasons for these differences are biological, psychological, and sociocultural,” psychology instructor Meghan Roarty said.
Despite this, the age of first diagnosis is typically higher for women than men (Nature). Additionally, women are more likely to be treated with minor tranquilizers and sedatives rather than analgesic pain medicine (Time). Women’s pain is more likely to be blamed on an emotional or psychological cause as opposed to a bodily or biological one.
“In medical school, there should be mandatory training in aspects of women’s health that are relevant to the field,” Elle Murata, a Ph.D. student studying neuroendocrinology said.
In her lab at UCSB, Murata studies the intersection of women’s health and neuroscience. She uses brain imaging tools to understand how the brain is shaped by sex hormones (estrogen, progesterone, and testosterone) across the lifespan.
In particular, she is interested in the impact of endometriosis and menopause on the brain.
“At the clinical level, we tend to think that ovarian hormones just act locally for reproduction, but they actually affect the entire body, including the brain,” Murata said.
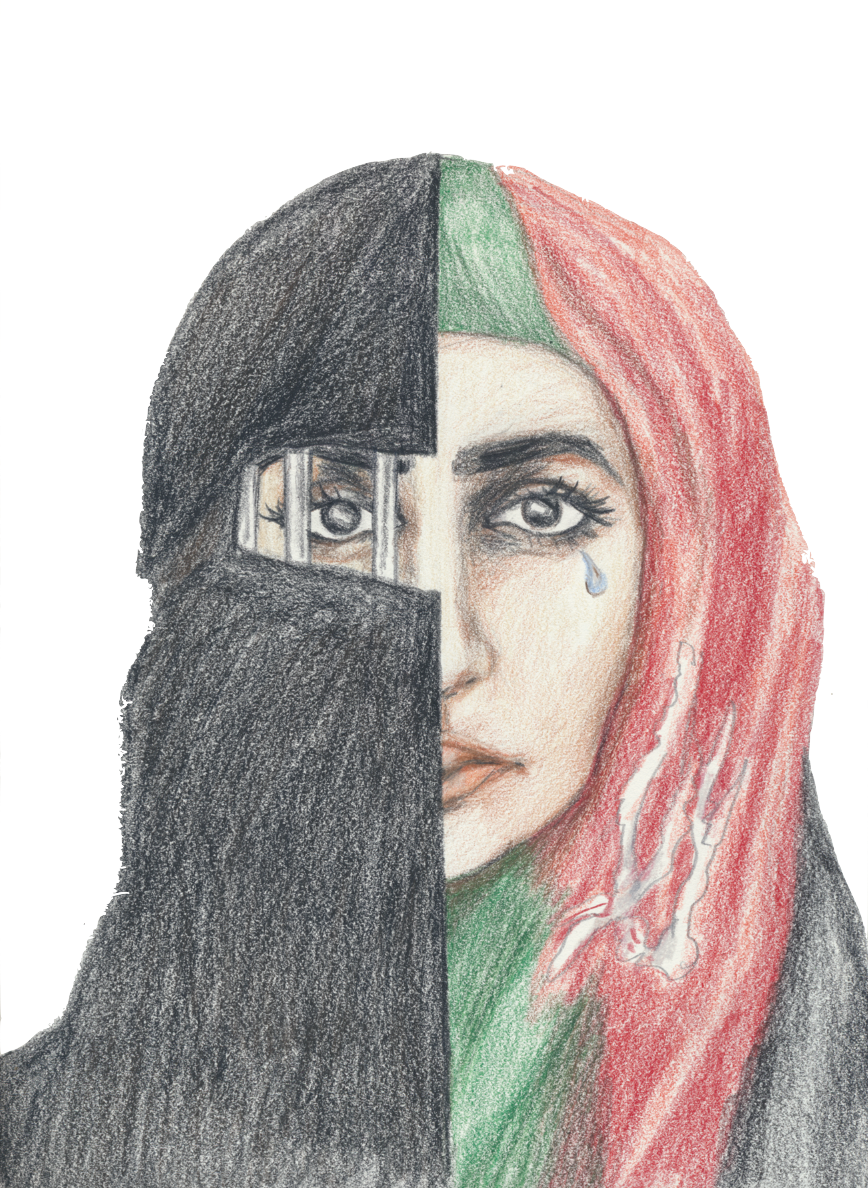
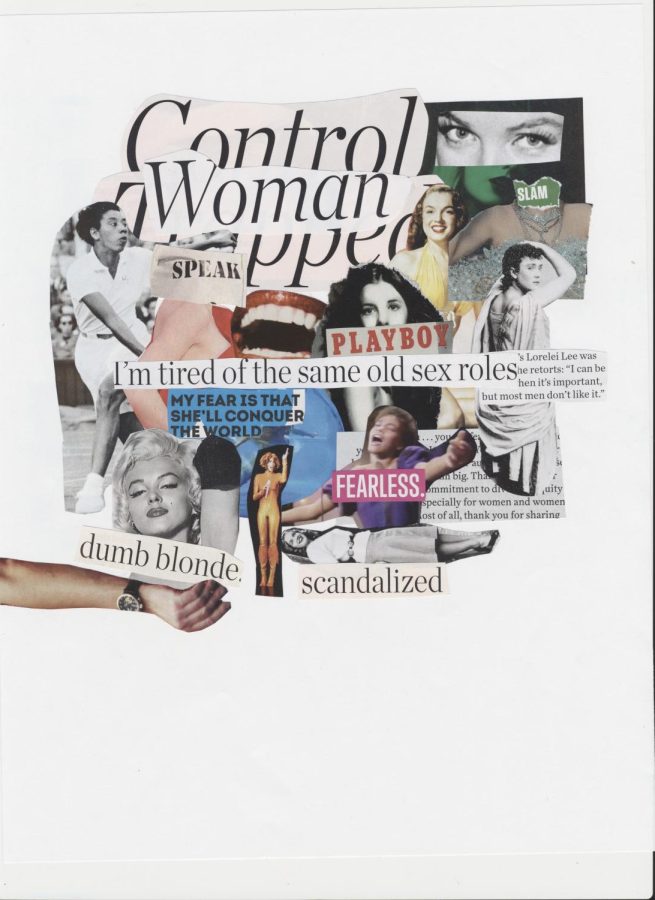
Since the dawn of time, women’s health has come second to men’s.
Women’s hormones were considered to be too unreliable and their bodies too weak to handle the plights of medical trials.
Because of this stereotype, the medical field lacks information about how women’s bodies handle certain medications and how diseases present in women.
“A lot of pain research has been conducted on rats, but that research is with some flaws, as the vast majority of those studies has only tested male rats, up until recently. This is greatly important given the role of hormones in experienced pain,” Roarty said.
Cancer and heart disease symptoms vary between men and women, but most of the time, the only symptoms women are told to look for are those present in their male counterparts.
As medicine developed in ancient Greece, the female body was considered an inverted male body; the only distinct importance was the womb because of its ability to bring new life into the world.
The possibility of further exploring women’s health was looked down upon, and it was seen as an unnecessary attribute to a field where the male body was the norm.
These beliefs continue to negatively influence the medical field to this day.
“Historically, we can think about the educators, scientists, and people in power making decisions about classes and requirements. When you look at who has been asking the questions, it’s historically been white men,” Murata said. “Because men weren’t experiencing hot flashes, menopause, pregnancy, and periods; they couldn’t think about these things and how they affect the brain and medicine.”
Before 2016, the National Institute of Health did not even require consideration of sex as a biological variable in its studies.
Since studies suggest that women are more likely to experience and express pain, medicine continues to ignore and dismiss female pain as psychological hysteria instead of addressing its chronic roots.
“In terms of social stereotypes, some studies have found that a woman’s reported pain is not taken as seriously as a man’s. These studies involved women and men expressing the same amount of pain, but participants in the study perceived the men’s pain to be more intense than that of the women’s pain,” Roarty said. “These types of studies have major implications for suggested treatments, such as prescribing medication versus psychotherapy.”
For example, the painful procedure of an IUD insertion is done without painkillers, and often, the cries of women’s intense pain during childbirth are ignored even if the IV bag has run out of painkillers.
“Psychologically, one area of research found that catastrophizing experiences, where pain signals get magnified and ruminated upon, are associated with increased sensitivity to pain. Women tend to engage in catastrophizing more often than men,” Roarty said.
The narrative that women are just being dramatic is especially visible in the diagnosis of painful periods, endometriosis complications, or migraines, where female patients are told that they have normal symptoms that they must tolerate and simply deal with. In reality, these symptoms can lead to severe illness and life complications.
“Birth control is slapped onto a problem whether it be missed periods from exercising or missed periods from a condition,” Murata said. “The issue is that we don’t talk about the side effects.”
Hormonal birth control works by adding hormones to correct an imbalance.
However, these hormones are different from the natural hormones produced by the body. These hormones don’t just have a localized effect; there are receptors in the brain specifically designed for them.
A 2016 study in Denmark found that when women take birth control, they have an increased chance of being diagnosed with depression.
Often, women are prescribed these life-altering medications with little information on how their bodies and minds will change.
The likely possibility of still having an undiagnosed issue that persists in the background of hormonal shifts is ignored.
“Some research has found that high levels of progesterone are correlated with pain reduction. When progesterone levels are high, women report less experienced pain and reduced pain intensity. Testosterone also appears to be correlated with pain reduction, which may be one reason why men overall may experience less pain,” Roarty said.
Birth control being used as a patch fix for problems females experience links to a greater issue of dismissing female issues as trivial.
“There are problems you could be ignoring or failing to treat when you are prescribed birth control. It’s given out so easily that you may not even know if you have Polycystic Ovary Syndrome (PCOS) like me. The same could be said for people with endometriosis who have chronic pelvic pain, so they are given birth control. There are many ways we could better educate people about the consequences,” Murata said.
Racial biases also play a significant role in properly diagnosing chronic pain, especially for women.
Doctors are more likely to ask Black and Hispanic women expressing their pain about their housing situation and financial status when compared to white women.
Only 35% of women ages 40-64 say their healthcare provider ever talked to them about what to expect in menopause (kff.org), and 8% more women than men aged 18-64 reported their doctor dismissed their concerns between 2021 and 2022.
“We are doing some really cool work with pregnancy right now that shows the brain changes at the structural and functional level with changing hormones. This is likely related to the fine-tuning of the brain to prepare for the new territory that is parenthood,” Murata said. “Through our work, we are trying to shape sex hormones as not a nuisance, burden, or something to be ashamed of, but something to be proud of.”
“It’s All in Your Head”
The medical field is unprepared for Women’s Health issues.
Lucia Camp, News Editor
March 21, 2024
0
Donate to The Fourth Estate
$50
$500
Contributed
Our Goal
Your donation will support the student journalists of Laguna Blanca School. Your contribution will allow us to purchase equipment and cover our annual website hosting costs.
More to Discover
About the Contributor

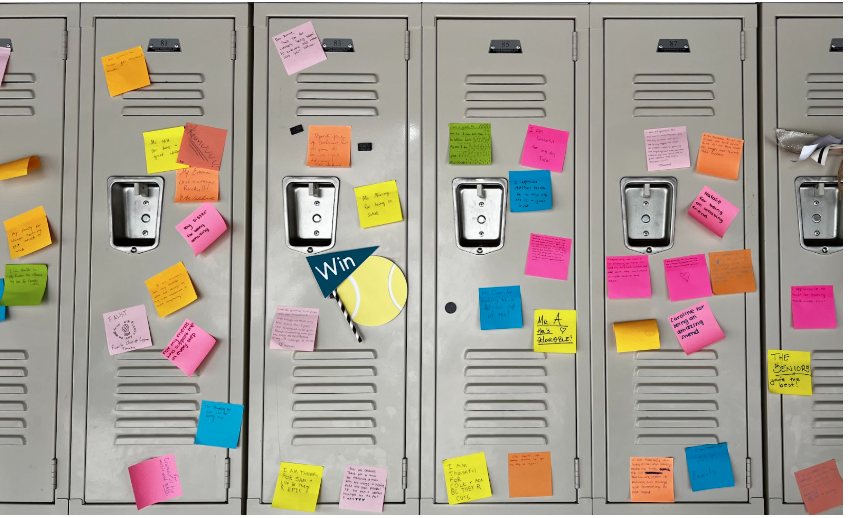
Lucia Camp, Co News Editor
Lucia Camp is a senior and second-year journalism student. Lucia's hobbies include cooking, hiking, paddleboarding, yoga, and sewing. Lucia enjoys playing tennis and spending time with loved ones. She is also a member of the Laguna mock trial team. She has interests in criminal and social justice, local issues, and environmental science and is an active member of the Santa Barbara Youth Council.